cranial protective device
Background
Severe stroke and traumatic brain injury (TBI) patients often need to undergo a decompressive craniectomy, where a portion of the skull is removed to alleviate intracranial pressure. These patients then require a cranioplasty to repair the skull. This procedure is often performed weeks or months after the craniectomy. An estimated 20 million decompressive craniectomies are performed each year.
69 MILLION
6.2 MILLION
individuals suffer TBIs each year
people died from stokes in 2019 alone
Traumatic brain injuries are 3x more common in low- and middle-Income countries (LMICS)
TBI Causes
1. Decompressive Craniectomy
A portion of the skull is removed to alleviate intracranial pressure and prevent imminent neurological damage.
2. Interim Period
In between the decompressive craniectomy and reconstructive surgery, the patient is at an increased risk while the brain is left largely unprotected.
3. Cranioplasty
The portion of the skull is then reconstructed after pressure/swelling has subsided.
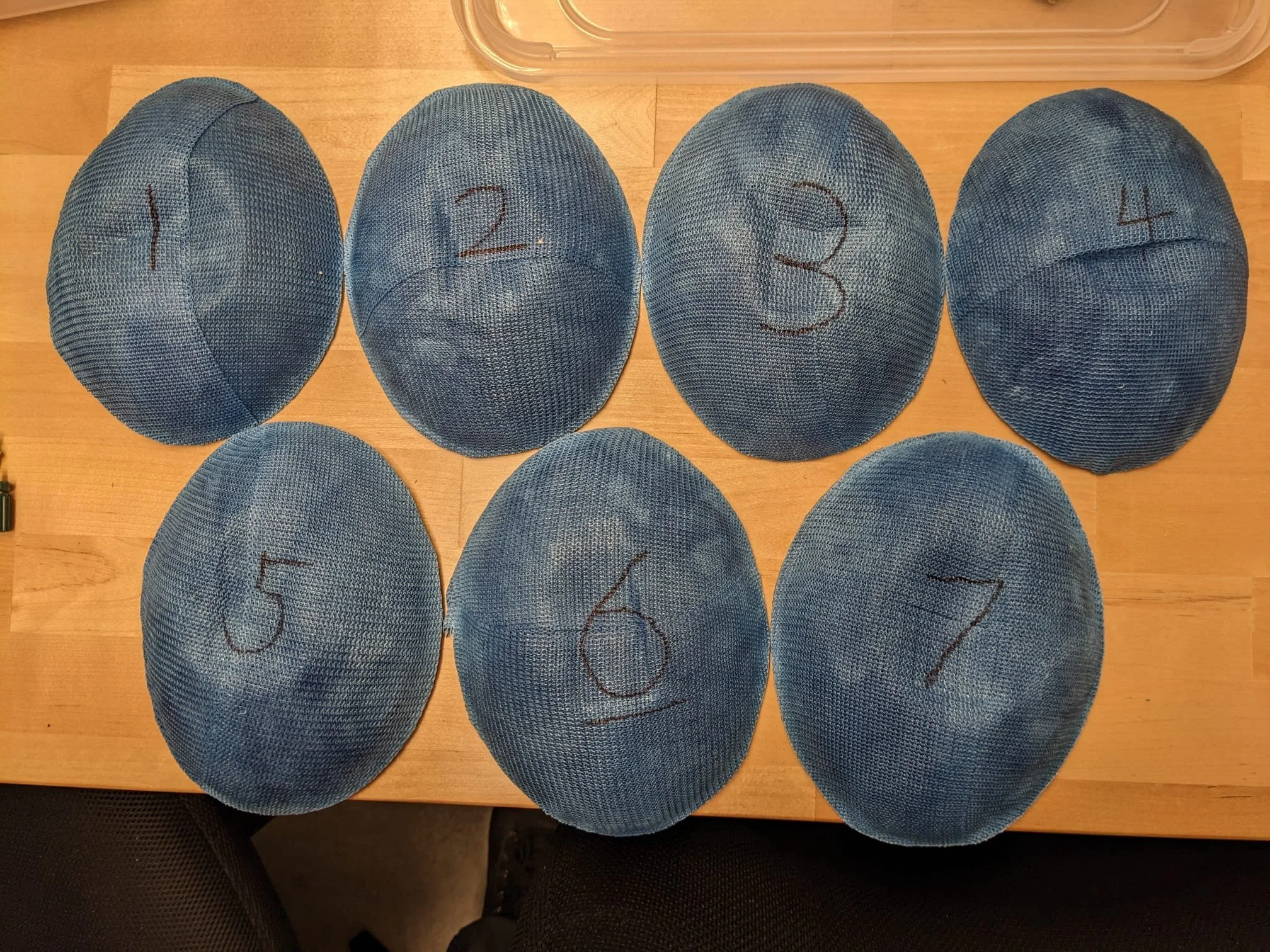
The Team
I worked on an international, interdisciplinary team of students to address this challenge; spanning across design, engineering, and medical disciplines. On this team, I am responsible for ideating solutions based on research insights, refining the product experience, collaborating to design higher fidelity prototypes in CAD, printing, casting, and assembling 16/27 prototypes and conducting testing on them. As a part of this, I was responsible for evaluating the design's durability, assessing opportunities for cost reduction, and designing for human factors/anthropometric design.
Laura Fernandez, MD (left)
Master’s of Clinical Investigation Student — University of Utah
myself, Bennett Graff (right)
Industrial Design Student — Brigham Young University
Diana Rodriguez (middle left)
Mechanical Engineering Student — Universidad Metropolitana, Caracas
Han Wu (middle right)
Biomedical Engineering Student — University of Utah
Research
Our research going into this focused on interviewing neurosurgeons in LMICs (particularly in Colombia and Venezuela), getting the perspectives of patients on a more informal basis, and going through the pre-existing literature on how people have tried to address this issue in the past.
These perspectives brought to light issues that weren’t clearly articulated or prioritized in the literature, such as issues around patient psychological well-being through this process, which is influenced both by the traumatic disruption of body integrity and by the affects of prolonged exposure of the brain to atmospheric pressure.
We also were able to learn more about what the common practices are for protecting this operation site; in some cases, neurosurgeons will spend about an hour creating a plaster protective barrier around the site, but this solution has many issues around comfort, durability, and washability, not to mention how time-consuming it is to create. More often than not, these patients go totally unprotected for extended periods of time, putting them at great risk.
The Problem
Protective devices are cost-prohibitive in low- and middle income countries (LMICs); going unprotected puts patients at risk for permanent neurological damage
Patients in LMICs often go much longer between operations, often 3 months, sometimes more than a year, putting them at an even higher risk
This recovery period often affects a patient’s ability to work
Neurosurgeons and nurses are often forced to improvise protective solutions that are time-consuming to create, uncomfortable for patients, and difficult to clean.
Patients suffer negative psychosocial impacts due to disruption of body integrity both from having their heads shaved for the operation and from the operation itself.
Protective solutions have issues with product stigmaticity
Exploration
The unique shapes and sizes of each patient’s head provided an challenging design constraint; much of our early ideation was focused on creating protective devices that were unique to each patient.
We were also trying to address the unique challenge of creating negative pressure, which can help protect the brain from damage by atmospheric pressure.
Our continued research and co-creation with neurosurgeons in Colombia and Venezuela helped us realize that some of our initial assumptions we had were inaccurate.
We found that providing protection against atmospheric pressure could potentially be useful, but wasn’t a high priority for these neurosurgeons; they were most concerned with the cost-accessibility of having a physical barrier over the injury site.
Not only was this phase useful for brainstorming a variety of approaches, but it also was instrumental in articulating our concepts with enough fidelity to make our assumptions visible to the experts we were co-creating with. This helped to generate ideas and better understand the research and clinical needs.
Iterative Process
Early stage/low-fidelity Prototyping
High-Fidelity Prototyping
We chose to address the issue of being adaptable to each patient with mass production capability by over-molding a silicone cushion onto a plastic protective shell. This prototype was our first exploration of how to create this over-molded component and determine what durometer of silicone would be most appropriate to support the device while also prioritizing patient comfort (in this case 00-30)
Version 2
The second iteration of our main concept was a fully functional prototype. It featured the same plastic over-molded cushion which with this design was shown to be able to attach itself in place with suction. While we decided this wasn’t sufficient to secure it constantly, it significantly enhanced the workflow for applying and removing the device and enabled greater patient autonomy. This prototype also explored how straps would attach; here we decided to attach a removable ring where adjustable straps would attach. Breaking the device up into 2 separate components made it easy to apply because first it could be suctioned in place, and then secured in place with the straps, enabling the user to focus on one component at a time without trying to juggle both. We did find some weaknesses in the design such as the strap angles and the fact that it only worked to secure it on the left side; both issues that were addressed in the subsequent prototypes.
Version 3
This iteration of the prototype added an ergonomic feature to the protective shell and also reduced the material further, by making it thinner. This version also features a cushion that better grips the head, making for easier application.
Latest Design
Patient Experience
Patient psychosocial needs were a high priority. The combination of having to have their head shaved in advance of the procedures and the normal integrity of their skull being disrupted by the decompressive craniectomy can be a traumatic experience, even before getting into the stigma around the difference in physical appearance. That’s why our solution was designed to that it could be easily concealed under commonly worn head coverings.
Our method of strapping the device to the head doesn’t use a chin strap and avoids unnecessary product stigmaticity
Provider Experience
Our latest prototype iteration is fully functional. The strap attachment ring has been redesigned since the prototype before so it’s now reversible, and the same attachment mechanism will work on both the left and right sides.
Cost & Competitors
The A-Flex Plus™ Protective Headgear is a commonly prescribed protective helmet for patients in high-income countries such as the United States. It costs 307.45 USD, which can make it cost-prohibitive to uninsured patients and patients in low- and middle-income countries.
Our estimated manufacturing cost is around $5, and we anticipate being able to sell our product at $20-25 (15x cheaper than current competitors on the market) so we can make this accessible to LMIC patients.
Version 1
Validation
Bench to Bedside Competition
My teammates and I presented our work at the Bench to Bedside competition put on by the University of Utah’s Center for Medical Innovation at the Utah State Capitol. At this competition, we were able to connect with a number of people in the medical product industry who gave us feedback and were able to point us in new directions as we continued our work. Our concept was evaluated by a panel of about 20 industry-professional judges, and of the 27 teams competing, we were selected to get $5000 in funding for being the “Best in Business.”
Neurosurgeons in LMICs
“EXOCRANIO Se convierte en una craneoplastia externa cómoda, y sin duda es la mejor alternativa costoefectiva para pacientes de países de bajos y medianos ingresos. Al corregir de manera temporal el defecto de cobertura craneal, genera un gran impacto en la calidad de vida, sentido de la estética y estado de ánimo, pero sobre todo gracias a su gran desempeño funcional, le permite mitigar el efecto de la presión atmosférica sobre el cerebro y con ello en el síndrome del colgajo hendido.”
“EXOCRANIO becomes a comfortable external cranioplasty, and is without a doubt the best cost-effective alternative for patients from low and middle-income countries.
By temporarily correcting the defect of cranial coverage, it has a significant impact on the quality of life, cosmesis, and self-esteem, but above all else, thanks to its high functional performance, it’s able to mitigate the effect of atmospheric pressure on the brain and by extension the sinking skin flap syndrome (SSFS)”
Dr. Diana Marcela Sánchez Parra, Neurosurgeon UCMH, Neurotrauma/Neurocritical Care U. Cambridge
“The idea of having something protecting the brain in the craniectomy site I think it’s amazing. This prototype had [taken] everything into account, the comfort, the aesthetic, the functionality, and the economic factor. It’s especially useful in countries where the access to health services is limited, because it prevents complications for the patients. In countries like Colombia, where sometimes the cranioplasty will take longer than expected for administrative and access reasons, [it] is a great solution. I would definitely recommend this to my patients.”
Dr. Sarita Aristizabal, Neurosurgery PGY1 in Colombia